Press Release
Contact
Molly McDougall
HealthFlash Marketing
203-431-4000
molly@healthflashmarketing.com
Sharon Grutman
The American Society of Breast Surgeons
877-992-5470
sgrutman@breastsurgeons.org
Download
Reduced-Opioid Prescription Program Supports Effective Post-Operative Pain Management
- Abstract: Reducing Narcotic Prescriptions in Breast Surgery Patients: A Prospective Analysis
Dallas, May 2, 2019--A breast surgery opioid prescription management program, which analyzed current physician patterns and provided education and guidelines, successfully reduced the volume of narcotics given post-operatively to patients at a large institution in a new study presented this week at the annual meeting of the American Society of Breast Surgeons.
In the study, a baseline review of medication practices found lack of a clear standard for opioid prescriptions with highly significant variation across individual surgeons. Following a review with physicians about the median and range numbers of pills given for pain, opioids prescribed to patients for home use decreased significantly. A survey of patients revealed that they took even fewer pills than prescribed with a subgroup that took none at all.
“Prescribed narcotics add to today’s crisis,” says Stephanie Valente, DO, FACS of Cleveland Clinic and one of the study authors. “Overprescribed drugs can contribute to a problem for patients. Unused pills can also make their way into the general population. As physicians, we have an obligation to ensure opioids are not prescribed unnecessarily, but that post-operative pain is appropriately controlled. This prospective quality initiative study provided our breast surgeons the information to do so.”
In the study, researchers established a baseline by reviewing the opioids prescribed to 100 patients during a one month period in 2017. Following implementation of the surgeon education program, data was collected on new narcotic regimens. A patient follow up survey assessed the actual number of pills patients used.
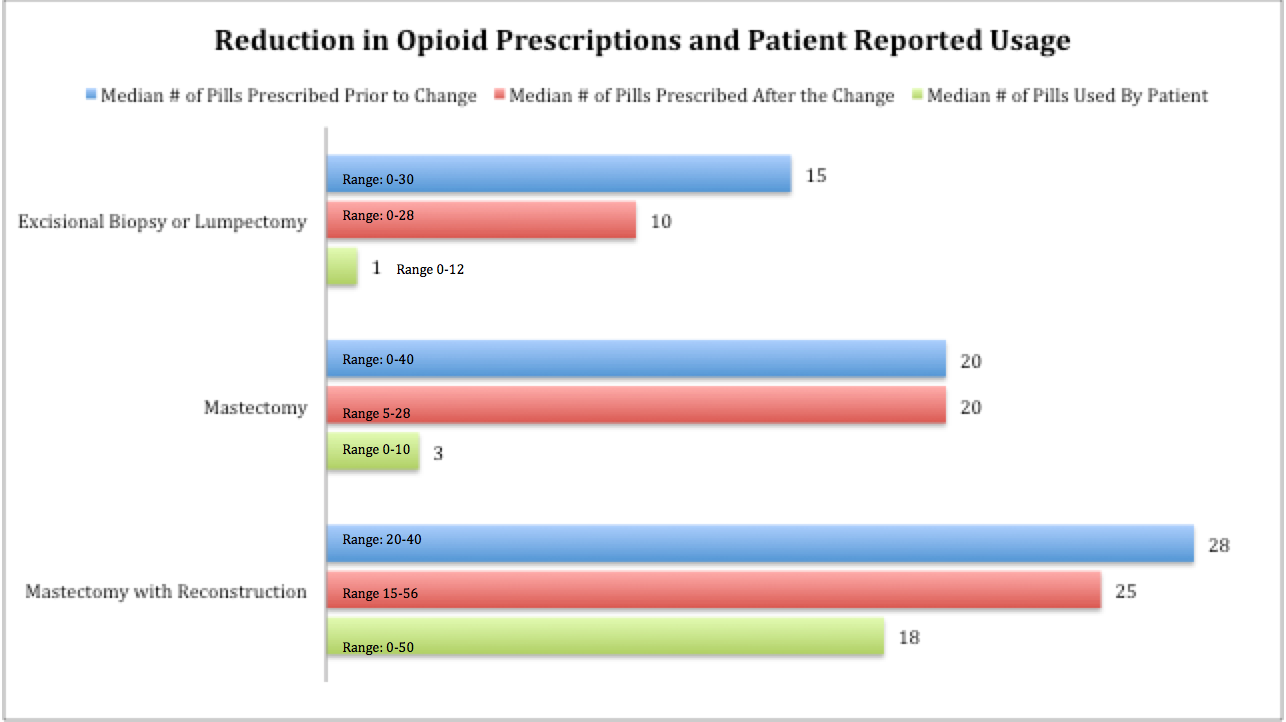
Prescribed opioids included Tramadol, Tylenol-3, Norco/Hydrocodone, and Percocet/Oxycodone and ranged from 0-40 pills. Prior to the program, the median pills number of pills given for excisional biopsy/lumpectomy was 15, mastectomy was 20, and mastectomy with reconstruction was 28. Planned modification of prescribing patterns resulted in a statistically significant reduction in the number of pills given to patients for excisional biopsy/lumpectomy with 10 (p<0.01) pills prescribed and mastectomy with reconstruction with 25 (p<0.01) pills prescribed. The median medication taken by patients was significantly less than prescribed. Forty percent of patients reported using no prescribed opiates.
“Little information exists in the literature about appropriate opiate dosing for post-operative breast surgery pain,” says Dr. Valente. “Many surgeons draw on their medical school backgrounds. Better physician education based on patient feedback is important to help address today’s opiate crisis. Patients are concerned with opioid medications and want to take the minimum amount needed, which is lower than physicians assume.”
Dr. Valente believes that an important next step will be analyzing why some patients are able to refrain from taking any narcotic medications and whether factors other than individual pain threshold account for the differences. She notes, “Alternatives to narcotics exist for post-surgical pain. Local anesthetics, nerve blocks, anti-inflammatory and anti-nausea medications and old fashioned icing all can help. Physicians must take stewardship of opioid prescribing habits and look for alternative medications which can work just as well.”
Expert Commentary:
This study will have a large impact as more than 500,000 breast surgeries are performed each year in the United States. This evidence-based approach for modifying procedure-specific pain medication prescribing practices by surgeons will help to balance patient comfort and safety.
Henry M. Kuerer, MD, PhD, FACS
University of Texas MD Anderson Cancer Center, ASBrS Publications Committee Co-Chair
Abstract, Official Proceedings
Reducing Narcotic Prescriptions in Breast Surgery Patients: A Prospective Analysis
Authors: Betty Fan, Stephanie Valente, Sabrina Shilad, Zahraa Al-Hilli, Diane Radford, Chao Tu, Stephen Grobmyer
Institutions: Cleveland Clinic, Cleveland, OH
Objective: Recent studies have shown that narcotics prescribed for postoperative pain may be overprescribed and result in excessive unused pills that could lead to potential abuse. No clear standard regarding number or type of narcotics for adequate postoperative pain control have been established for breast surgery. In this study, we aimed to review our opioid prescribing patterns, implement a change to reduce and standardize our prescribing practices, and evaluate the utilization of these narcotics for patients who underwent breast surgical procedures. The goal was to optimize the practice of post-operative narcotic prescribing in breast surgery patients.
Methods: In order to establish baseline prescribing practice, a review of consecutive breast surgical patients treated in 2017 was performed to establish baseline postoperative narcotic prescribing patterns. The most common medications prescribed and the number of pills given for excisional biopsy/lumpectomy, simple mastectomy, and mastectomy with reconstruction were documented. The median and range numbers of narcotics prescribed were then used to educate surgeons about prescribing patterns. Starting in February 2018, the department implemented a planned change based on our findings and reduced the number of narcotic pills prescribed. We then prospectively collected data on prescribing patterns and recorded how many pain pills patients actually took of those prescribed after discharge. Data regarding changes in the amount of narcotics prescribed and patient use patterns were analyzed.
Results: Baseline narcotic prescribing patterns from 100 consecutive breast surgery patients identified that narcotic prescribing practices were not consistent in either the type or number of narcotics prescribed. Narcotics prescribed included Tramadol, Tylenol-3, Norco/Hydrocodone, and Percocet/Oxycodone and ranged from 0-40 pills (Figure). The median number of narcotic pills given for excisional biopsy/lumpectomy was 15, mastectomy 20, and mastectomy with reconstruction 28. Following planned modification of prescribing patterns, review of 103 breast surgery patients identified a statistically significant reduction in the number of narcotic pills prescribed for excisional biopsy/lumpectomy (p<0.01) and mastectomy with reconstruction patients (p<0.01). Even after the prescribing reduction, the median number of narcotic pills taken by patients was significantly less than that prescribed for patients in all categories: 1 pill for excisional biopsy/lumpectomy, 3 pills for mastectomy and 18 pills for mastectomy with reconstruction (p<0.01, p<0.01, p<0.01 respectively). 40% of our sampled patients reported using zero prescribed narcotics after their operation.
Conclusions: A narcotic prescribing reduction program can be successfully implemented in breast surgery patients. Half of patients undergoing excisional breast biopsy, partial mastectomy and mastectomy without reconstruction used less than 3 pills after hospital discharge. These observations regarding narcotic use in breast surgery patients can be used to further optimize narcotic prescribing practices in these patients.