Media Tip Sheet
Contact
Molly McDougall
HealthFlash Marketing
203-431-4000
molly@healthflashmarketing.com
Sharon Grutman
The American Society of Breast Surgeons
877-992-5470
sgrutman@breastsurgeons.org
Download
Additional Notable Research Presented at the 20th Annual Meeting of the American Society of Breast Surgeons
The following newsworthy abstracts presented at the 20th Annual Meeting of the American Society of Breast Surgeons (ASBrS) may be of particular interest to press, in addition to presentations during the Media Press Briefing. Researchers are available for telephone interviews. Onsite media is invited to attend all scientific sessions.
Abstracts
- Abstract: Is Routine Oncotype Testing in Patients Over 70 Years of Age Warranted? An Evaluation of the National Cancer Data Base after TAILORx
Lead Author: Rachel Lee, MD
Winship Cancer Institute, Emory University
Atlanta, GA - Abstract: A Comparison of Patient-Reported Outcomes after Breast-Conserving Surgery and Mastectomy with Implant Breast Reconstruction
Lead Author: Meghan Flanagan, MD
Memorial Sloan Kettering Cancer Center
New York, NY - Abstract: Burnout and Professional Fulfillment in Breast Surgeons
Lead Author: Jennifer Zhang, MD
Beth Israel Deaconess Medical Center
Boston, MA
ATTRIBUTION TO THE 20th ANNUAL MEETING OF THE AMERICAN SOCIETY OF BREAST SURGEONS IS REQUESTED IN ALL COVERAGE.
Abstract, Official Proceedings
Is Routine Oncotype Testing in Patients Over 70 Years of Age Warranted? An Evaluation of the National Cancer Data Base after TAILORx
Authors: Rachel Lee1, Jeffrey Switchenko2, Tran Ho1, Cletus Arciero1, Manali Bhave3, Preeti Subhedar1
Institutions: 1Winship Cancer Institute, Division of Surgical Oncology, Department of Surgery, Emory University, Atlanta, GA, 2Winship Cancer Institute, Biostatistics and Bioinformatics Shared Resource, Emory University, Atlanta, GA, 3Winship Cancer Institute, Department of Hematology and Medical Oncology, Emory University, Atlanta, GA
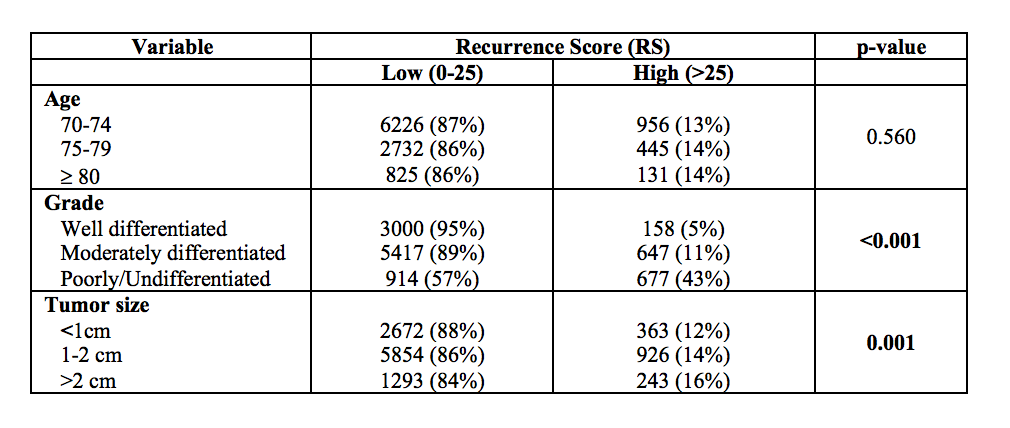
Objective: Oncotype testing in early-stage, hormone-positive breast cancers is used to predict the benefit of adjuvant chemotherapy for disease recurrence and overall survival (OS). Application of TAILORx results decreased the ambiguity of an “intermediate risk” recurrence score (RS) by stratifying scores into a binary classification system. Our aims were (1) to determine how women >=70 years with previously deemed intermediate RS were redistributed using post-TAILORx classification and (2) to identify predictors of high RS, based on TAILORx classification, in patients >=70 using a large national database.
Methods: Patients >=70 years with early-stage, node-negative, ER-positive, HER2-negative breast cancers who underwent oncotype testing in the National Cancer Database (2004-14) were included. Oncotype scores were defined in 2 ways: “pre-TAILORx” scores were classified into low (0-18), intermediate (19-30), and high risk (>30) groups; “post-TAILORx” scores were classified into low (0-25) and high risk (>25) groups.
Results: A total of 11,355 women were included. The average age was 74 years. Using pre-TAILORx classification, 61% (n=6967) were low risk, 31% (n=3546) were intermediate risk, and 7% (n=842) were high risk. Using post-TAILORx classification, 14% (n=1532) were high risk. Of the 3546 patients previously deemed intermediate risk, 81% (n=2856) were reclassified as low risk and unlikely to benefit from chemotherapy. As expected, only 11% (n=1217) of patients in this elderly cohort received chemotherapy. Of the patients classified as intermediate risk prior to TAILORx who received chemotherapy, 10% (n=289) would have been spared chemotherapy by being reclassified into the low-risk classification after TAILORx. The strongest predictor of post-TAILORx low-risk RS was tumor grade; 95% of well-differentiated tumors and 89% of moderately differentiated tumors had a low-risk RS, compared to 57% of poorly/undifferentiated tumors (p<0.001). Smaller tumor size was also predictive of low-risk RS. Age was not associated with RS (Table).
Conclusions: With new TAILORx criteria for oncotype stratification, the vast majority of patients >=70 can be classified as low risk and thus unlikely to benefit from chemotherapy. The majority of cancers in this cohort were well differentiated and associated with a low-risk RS. Given that this age group has a greater rate of chemotherapy associated complications, increasing the risks of unnecessary treatment, and considering increased health care costs associated with testing, reconsideration of routine oncotype testing in patients >=70, especially in those with well-differentiated tumors, is warranted. We propose that the decision to use oncotype testing be individualized in this elderly cohort. In addition to taking into account functional status and ability to tolerate chemotherapy, tumor grade and size may also better inform the decision to omit using oncotype score, especially in elderly patients with well differentiated tumors.
Abstract, Official Proceedings
A Comparison of Patient-Reported Outcomes after Breast-Conserving Surgery and Mastectomy with Implant Breast Reconstruction
Authors: Meghan Flanagan1, Emily Zabor2, Anya Romanoff1, Sarah Fuzesi1, Michelle Stempel1, Babak Mehrara3, Monica Morrow1, Andrea Pusic4, Mary Gemignani1
Institutions: 1Breast Service, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York, NY, 2Biostatistical Service, Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center, New York, NY, 3Plastic and Reconstructive Surgical Service, Memorial Sloan Kettering Cancer Center, New York, NY, 4Division of Plastic Surgery, Brigham and Women’s Hospital, Boston, MA
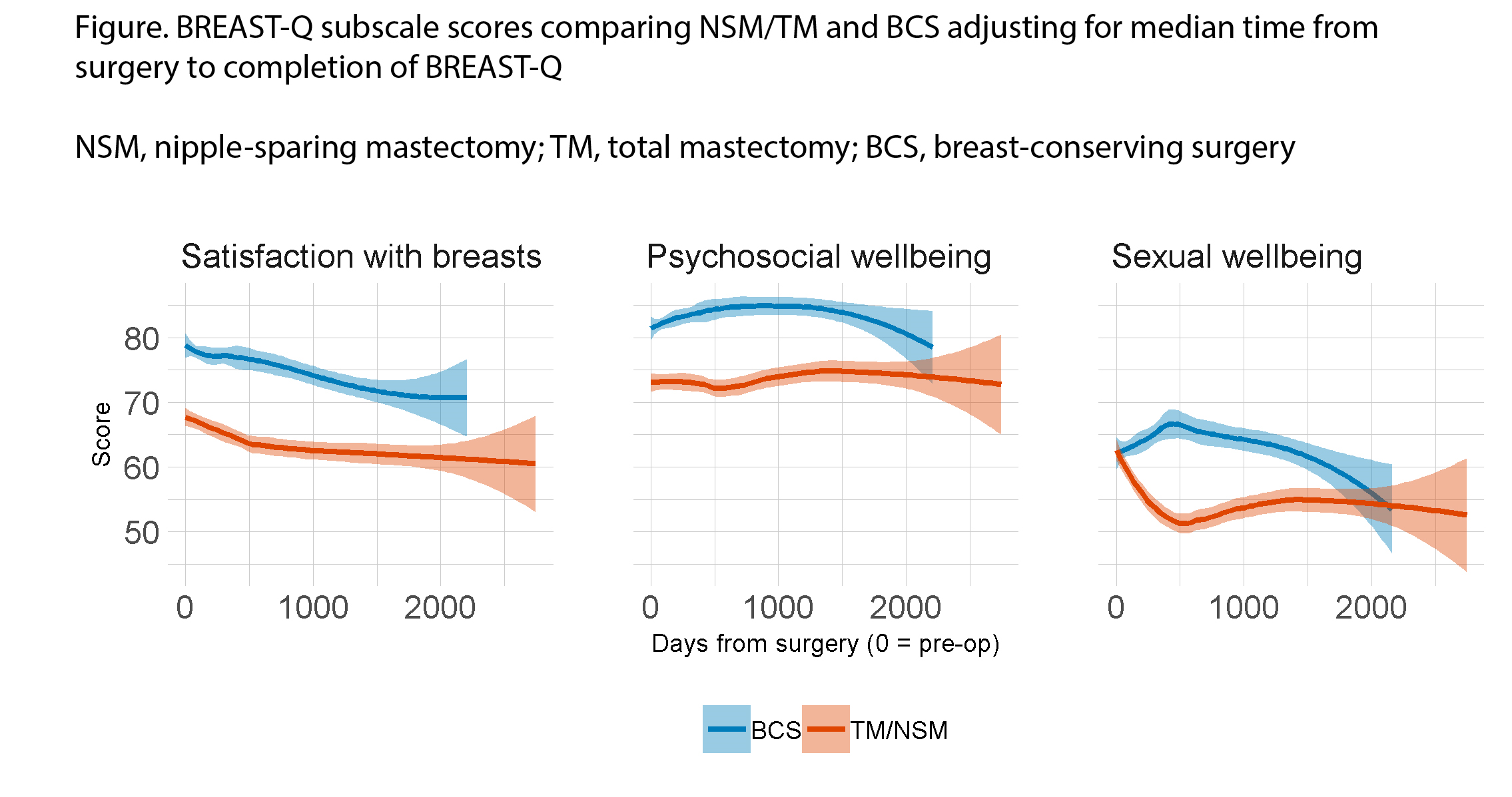
Objective: Many factors influence decisions regarding choice of breast-conserving surgery (BCS) versus mastectomy with reconstruction for early invasive breast cancer (BC). The purpose of this study was to compare patient satisfaction following BCS and mastectomy with implant reconstruction utilizing the BREAST-Q patient-reported outcome measure.
Methods: Women with stage I or II BC undergoing BCS or nipple-sparing (NSM)/total mastectomy (TM) with immediate tissue expander/implant reconstruction who completed a BREAST-Q from 2010 to 2017 were identified by retrospective review of a prospective database. Baseline characteristics were compared, and linear mixed models were used to analyze associations with BREAST-Q scores over time.
Results: Our study group comprised 3233 women; 2026 (63%) had BCS, 123 (3.8%) had NSM, and 1084 (34%) had TM. With BCS, 92% received radiation compared with 23% of NSM/TM (p<0.001). The median time from surgery to BREAST-Q was 205 days for BCS and 639 days for NSM/TM (p<0.001). The median age of the cohort was 53 years (range 23-97). Women who received BCS were older, more likely to have Stage I breast cancer and receive radiation therapy, and less likely to have chemotherapy (all p<0.001) compared with NSM/TM. Multivariable analysis included time from surgery, type of surgery, age, bilateral disease, any axillary procedure, path stage, chemotherapy, radiation, and conversion to mastectomy. Regardless of type of surgery, breast satisfaction scores decreased significantly over time (p<0.001) whereas psychosocial (p=0.001) and sexual (p=0.004) wellbeing scores increased significantly over time. BCS was associated with significantly higher scores over time as compared with NSM/TM across all subscales (all p<0.001) (Figure). Radiation was significantly associated with decreased scores over time across all subscales (all p<0.05). Older age (p<0.001) and Stage II vs I (p=0.001) were also associated with decreased breast satisfaction over time. Younger age (p=0.001) and Stage II vs I (p=0.031) were additionally associated with decreased psychosocial wellbeing over time. Chemotherapy (p=0.005) was associated with decreased sexual wellbeing over time. In a sensitivity analysis separating NSM and TM, NSM did not differ significantly from TM with respect to any of the subscales.
Conclusions: Although we noted significant differences in patient and disease characteristics among women who had BCS compared to mastectomy, on multivariable analysis, BCS was associated with significantly higher BREAST-Q scores. As expected, treatment-related factors such as radiation have a significant effect on breast satisfaction, and on psychosocial and sexual well-being. These findings may help in counseling women who have a choice for surgical treatment. Breast satisfaction scores decreased over time in all women, highlighting the need for further evaluation with longer follow-up.
Abstract, Official Proceedings
Burnout and Professional Fulfillment in Breast Surgeons
Authors: Jennifer Zhang, Luis Riba, Leo Magrini, Aaron Fleishman, Ted James
Institution: Beth Israel Deaconess, Boston, MA
Objective: Physician burnout is a well-recognized problem in health care that negatively impacts physician well-being and decreases the quality of patient care. Rates of professional burnout in breast surgery are not well defined. We sought to better understand the degree of burnout among breast surgeons and identify factors that may influence levels of burnout and professional fulfillment.
Methods: All United States members of the American Society of Breast Surgeons (ASBrS) with a valid email address (2568 surgeon members) were surveyed in October 2017. Results were anonymous, and participants were blinded to the study hypothesis. The survey consisted of 39 questions including demographic characteristics, practice patterns, and elements of the Professional Fulfillment Index (PFI). The presence of professional fulfillment was set at a score of 3.0 or greater, and the presence of overall burnout was set at 1.33 or greater, as previously published. Multivariable linear regressions were performed for overall burnout and professional fulfillment.
Results: Of the 2,568 surveys delivered, 708 surveys were initiated, and 660 were completed. The mean age of surgeons was 51.5 years, 68.6% were female, 86.4% were in a partnered relationship, and mean years in practice was 18.5 years. The majority worked 40-60 hours per week (median days worked per week was 5). Surgeons spent an average of 80% of work hours on patient care, and 64.8% had a full-time breast surgery practice; 51.7% practiced in a private setting, and 44.3% practiced in a population of 500,001 or greater. Overall, 270 (41.3%) of surgeons had evidence of burnout, and 379 (57.5%) did not have professional fulfillment. On multivariable analysis, years in practice was negatively associated with burnout, and working >60 hours per week was positively associated with burnout. Years in practice was positively correlated with professional fulfillment and having <50% of practice dedicated to breast surgery correlated negatively with fulfillment.
Conclusions: We identified that 41% of breast surgeons had burnout, and 57.5% did not have professional fulfillment. Our data suggest that specific clinical practice conditions largely influence rates of burnout and professional fulfillment. The risk factors identified in our analysis may be useful in identifying breast surgeons who are particularly at higher risk for burnout, and designing targeted interventions focused on the clinical practice environment to promote professional sustainability.