View the up-to-date information for the 2026 Annual Meeting.

Press Release
Contact
Molly McDougall/
Jeanne-Marie Phillips
HealthFlash Marketing
203-977-3333
molly@healthflashmarketing.com
Sharon Grutman
The American Society of Breast Surgeons
877-992-5470
sgrutman@breastsurgeons.org
Download
Positive Lymph Nodes Not an Indicator for Chemotherapy in Older Breast Cancer Patients
New Study Examines Correlation of Node Status with 21 Gene Recurrence Score
- Abstract: Oncotype DX scores and Nodal Status in Patients over 70 years old – Continue to Choose Wisely
Las Vegas, April 6, 2022—Positive lymph node status is not a reliable indicator of the need for adjunctive chemotherapy, and sentinel node biopsy may be unnecessary in older women with certain low-risk cancers, according to a new study presented this week at the American Society of Breast Surgeons annual meeting. The study examined the correlation between nodal status and 21 gene recurrence score, which reflects a tumor’s individual biology and is considered among the most reliable tools for chemotherapy decision-making.
While 2016 Choosing Wisely® guidelines advise against performing sentinel node biopsies on women 70 years of age or older with hormone receptor positive breast cancer, studies show physicians continue to do so for 65-85% of patients. Lead study author Katharine Yao, MD, Vice Chair of Research, NorthShore University Health System and Clinical Professor of Surgery at the Pritzker School of Medicine, University of Chicago, hypothesized that one reason surgeons continue to perform sentinel node biopsy on this patient population is to obtain nodal status for adjuvant chemotherapy decisions. However, the study found that regardless of their nodal status, a similar proportion of these women had 21 gene recurrence scores qualifying them for adjuvant chemotherapy.
Using the National Cancer Database, researchers analyzed 28,338 patients 70 years of age and older who were treated for HR+, HER2-, AJCC clinical stage T1-T2 breast cancers between 2010 and 2018. They examined the correlation of nodal status with 21 gene recurrence results and also identified other clinical and demographic factors associated with high 21 gene recurrence scores and the need for chemotherapy. Of the patients studied, 5,640 (19.9%) were node positive and 22,698 (80.1%) were node negative on pathology examination. Overall, the proportion of patients with a 21 gene recurrence score greater than or equal to 26 was 3,330 (13.1%) for node negative patients and 740 (14.7%) for node positive patients. A score equal to or greater than 26 typically indicates that chemotherapy will be beneficial.
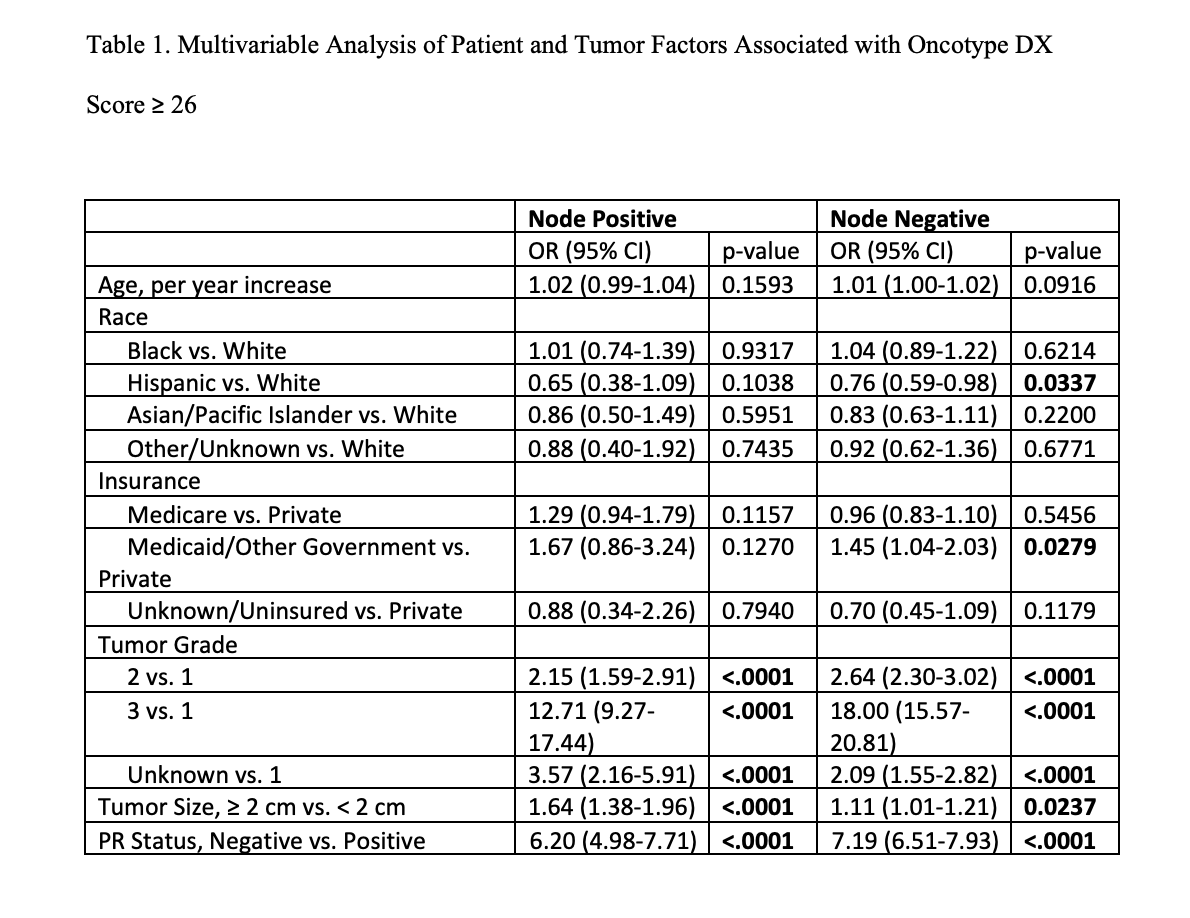
For both node negative and positive patients, a grade 3 tumor was associated most strongly with a high 21 gene recurrence score. Following this was negative progesterone receptor status. Additionally, women with tumors greater than 2cm and patients covered by Medicaid also were more likely to have a cancer recurrence score greater than or equal to 26. Hispanic patients were less likely to have a 21 gene recurrence score qualifying them for chemotherapy compared to Black and Asian women.
“Sentinel node biopsy has some associated morbidity and is an additional procedure in the operating room,” says Dr. Yao. “However, it may not provide the necessary information for decision-making about adjuvant chemotherapy. For this patient population, consideration of other tumor factors including possibly an Oncotype score may be more useful than nodal status.”
“Women may request sentinel node biopsies because cancer that has spread to the lymph nodes has become virtually synonymous with poor prognosis in the popular media,” notes Dr. Yao. “However, we are learning that there is more to tumor biology then just nodal status. Sentinel node biopsy for women older than age 70 with hormone receptor positive breast cancer is not really helpful for making adjuvant chemotherapy decisions. While eliminating sentinel node biopsy may seem counter-intuitive to some patients, it is not likely to have a major impact on their outcomes.”
Abstract, Official Proceedings
Oncotype DX recurrence scores and Nodal Status in Patients over 70 years old – Continue to Choose Wisely
Authors: Kyra Nicholson1, Anna Chichura2, Kristine Kuchta3, Catherine Pesce1, Katherine Kopkash1, Katharine Yao3
Institutions: 1NorthShore University HealthSystem & University of Chicago, Evanston, IL, 2University Of Chicago, Chicago, IL, 3NorthShore University HealthSystem, Evanston, IL
Objective: According to Choosing Wisely Guidelines, women > 70 years old with clinically node negative, hormone receptor positive (HR+) AJCC clinical stage I breast cancer do not need axillary sentinel node biopsy routinely. However, some clinicians may want nodal staging information for adjuvant therapy decisions. The Oncotype Dx breast recurrence score was developed to assess the need for adjuvant chemotherapy in addition to hormonal therapy. The objective of this study was to examine the distribution of the Oncotype Dx breast recurrence scores in women > 70 years old with HR+ AJCC clinical stage I breast cancers and identify clinical factors associated with a high recurrence score in this patient population.
Methods: Using the National Cancer Data Base we examined patients > 70 years old treated for HR+, HER2- breast cancers from 2010-2018. We dichotomized the Oncotype Dx scores into <26 and ≥26 based on prospective studies demonstrating benefit for adjuvant chemotherapy for scores ≥26 in this patient population. We compared the distribution of Oncotype scores between pathologically node positive and node negative patients. Multivariable logistic regression adjusting for patient and tumor and factors was used to determine factors associated with an Oncotype Dx score ≥26 for pathologically node negative and node positive patients.
Results: Of 28,338 patients 5,640 (19.9%) were node positive and 22,698 (80.1%) were node negative on pathology. Overall, the proportion of patients with an Oncotype Dx score ≥26 was 3,330 (13.1%) for node negative patients and 740 (14.7%) for node positive patients. Between 2010 and 2018, the proportion of patients with Oncotype Dx scores ≥26 remained stable at 13.1% in 2010 and 13.5% in 2018 but decreased from 20.0% in 2010 to 15.2% in 2018 for node positive patients. The strongest independent factor associated with an Oncotype Dx score ≥26 was tumor grade 3 for both node positive (OR 12.71 [95% CI 9.27-17.44], p<0.0001) and node negative (OR 18.00 [95% CI 15.57-20.81], p<0.0001) patients (Table 1). The second strongest factor was negative progesterone receptor status (OR 6.20 [95% CI 4.98-7.71, p<0.0001] node positive vs. OR 7.19 [95% CI 6.51-7.93, p<0.0001] node negative). Patients with larger tumors (> 2cm) and those on Medicaid were also more likely to have an Oncotype DX score ≥26. Hispanic patients were less likely to have an Oncotype DX score ≥26 when compared to other minority patients (Black and Asian), (OR 0.65 [95% CI 0.38-1.09, p 0.1038] Hispanic vs (OR 1.01 [95% CI 0.74-1.39, p 0.1593] Black vs (OR 0.86 [95% CI 0.50-1.49, p 0.5951] Asian node positive patients.
Conclusions: A similar proportion of women 70 with AJCC Stage I HR+, HER2- breast cancer have Oncotype DX scores ≥26 regardless of their nodal status. These findings suggest that sentinel node biopsy may not be helpful for adjuvant chemotherapy decisions in this patient population, but certain tumor factors may be more helpful.