Press Release
Contact
Molly McDougall
HealthFlash Marketing
203-431-4000
molly@healthflashmarketing.com
Sharon Grutman
The American Society of Breast Surgeons
877-992-5470
sgrutman@breastsurgeons.org
Same-Day Mastectomy Home Recovery Programs Benefit Patients with No Increased Risks
- Abstract: Same-Day Surgery for Mastectomy Patients in Alberta: A Perioperative Care Pathway and Quality Improvement Initiative
- Abstract: Implementation of Post-Mastectomy Home Recovery Program in a Large, Integrated Health Delivery System
Dallas, May 2, 2019--Comprehensive post-operative mastectomy home recovery programs significantly increased same-day patient discharge with no decrease in quality-of-care in two new studies presented this week at the annual meeting of The American Society of Breast Surgeons.
“Research demonstrates the safety of same-day home recovery for well-chosen mastectomy patients. Yet, utilization remains low,” comments Brooke Vuong, MD of Kaiser Permanente South Sacramento Medical Center, lead author of one study. “Many women feel more comfortable recuperating in a familiar environment, and risks of hospital acquired conditions are reduced, while inpatient resources are available for higher acuity patients.”
May Lynn Quan, MD of University of Calgary, lead author of the second study, notes, “Wound pain, shoulder movement and some psychological healing have demonstrated superiority in a home environment. With proper education and support many patients can recover and return to normal activities more quickly.”
With a government mandate to provide consistent quality-of-care and enhanced patient experience in 13 hospitals throughout the Canadian province of Alberta, Dr. Quan and her team developed a program to support home recovery as the standard-of-care for all mastectomy patients. The multi-pronged approach provided patient education about the care journey from diagnosis to survivorship with special emphasis on post-surgical expectations and potential problems as well as pathways to access clinical feedback and care.
A mastectomy education booklet, group classes and online resources also were developed for patients and families. From pre-admission to operating and recovery room staff, the entire care team was educated about the program to ensure they understood the process and delivered consistent information.
“We found patients really wanted to go home following surgery,” says Dr. Quan. “They felt empowered to play an important role in their recovery, and hospital staff themselves became better informed about the mastectomy process.”
The program was developed and implemented across the province during an 18-month period. Data was collected for same-day patient discharge, emergency visits and readmission. Since implementation, home recovery participation has risen from 1.2% to 40% through 2018. Of the 102 patients participating in a voluntary post-operative survey, 91% indicated they felt “excellent or good” with the plan to go home, 93% felt “excellent or good” caring for themselves, and 93% felt “excellent or good” about knowing how to access support if needed. A standardized questionnaire designed to measure the quality of recovery one week following surgery on issues from pain management to the ability to eat, sleep and care for themselves, as well as general well-being and return to routines, found an average score of 7.9/10.
In 2017, The Permanente Medical Group initiated a mastectomy home recovery program across 21 medical centers with the goal of increasing home care and patient satisfaction. Single and double mastectomy, lymph node as well as immediate implant-based reconstruction cases were included. The program began with an initial pre-operative patient education session to teach skills such as drain care. The complete care team, from breast care coordinators to post-anesthesia care unit recovery nurses and nurse navigators, also received training. Best practices were shared regularly across all hospitals.
The study examined home care rates and quality-of-care measures for all women undergoing mastectomy for six months prior to and following program implementation. Prior to the program, 165 of 626 or 26% of mastectomies were outpatient procedures. Following implementation, 404 of 620 or 65% were home recovery. Despite the increase in home recovery, the study found no statistical differences in emergency visits, reoperation or readmission.
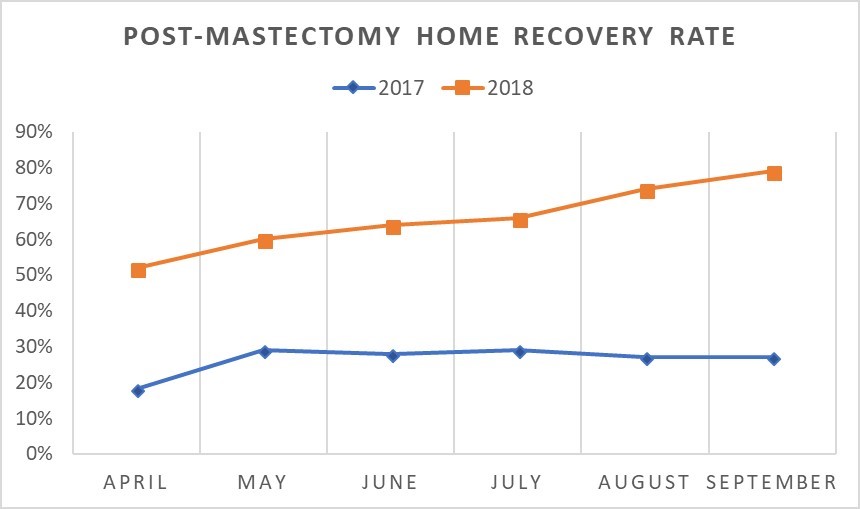
“Notably,” adds Dr. Vuong, “at study launch only 18% of mastectomies were outpatient, while during the last month in the study, the figure had risen to 79%. That reflects the tremendous satisfaction of all stakeholders in the program.”
Both surgeons agree that increasing post-mastectomy home care adoption is an important goal.
Expert Commentary:
The impetus behind these two significant quality-improvement studies was to allow patients to recover from surgery at home in a comfortable, familiar environment; to achieve a cost-savings compared to next day discharge after mastectomy; and to have more hospital availability for higher acuity patients. Both studies showed a significant increase in the number of patients discharged on the same day as mastectomy surgery compared to the pre-study baseline. Importantly, same-day discharge patient satisfaction was high. But researchers note that same-day discharge is not for every patient.
Jeffrey S. Falk, MD, FACS
Ascension Saint John Hospital, ASBrS Membership Committee Co-Chair
Abstract, Official Proceedings
Same-Day Surgery for Mastectomy Patients in Alberta: A Perioperative Care Pathway and Quality Improvement Initiative
Authors: Alysha Keehn1, David Olson2, Joseph Dort1, Shannon Parker3, Susan Anderes3, Lynn Headley3, Adam Elwi3, Angela Estey2, Alysha Crocker3, May Lynn Quan1
Institutions: 1University of Calgary, Calgary, AB, Canada, 2University of Alberta, Edmonton, AB, Canada, 3Alberta Health Services, Calgary, AB, Canada
Objective: Despite evidence supporting same-day surgery (SDS) for mastectomy with no difference in wound complications, readmission and reoperation rates compared to those admitted overnight, uptake of early discharge remains low in Alberta. In addition to being safe, SDS has been shown to improve shoulder movement, reduce wound pain and decrease anxiety with high patient satisfaction and expedited psychological recovery. Moreover, overnight admissions following mastectomy in medically and socially fit breast cancer patients is an inefficient use of acute care resources. In response to a national performance review highlighting SDS for mastectomy at 1% in Alberta, we developed and implemented a SDS pathway to improve the quality of perioperative care for women undergoing mastectomy. The objective of this study is to describe the development, implementation, rate of SDS, and patient-reported experience (PRE) measures for a quality improvement initiative supporting SDS for mastectomy.
Methods: A multi-tiered perioperative pathway for SDS was conceived and designed in 2015 supporting 3 main groups: surgeons/nurse navigators, perioperative nurses, and patients/caregivers. Implementation was carried out via 5 regional committees, each composed of 6-8 local members: breast surgeon, nurse navigator, and operational leads for each of the following areas: pre-admission, day surgery, inpatient unit, operating room, and post-anesthetic recovery room. Local present- and future-state opportunities along the patient care experience were identified for each region where specific steps could be taken to improve the utilization, safety, and support for patients having SDS. Provincially branded materials for surgeons/nurse navigators included formal SDS presentations, order set templates, and “standard operating” procedures with early nursing contact and plan for assessment outside of emergency services if a post-operative issue were encountered. Two dedicated nurse educators provided in-service teaching for each perioperative team at 13 hospitals across the province. This included provision of standardized drain care and discharge teaching forms. A patient education booklet, group teaching classes, and online resources were developed for patients and families. A measurement framework was created, and data were collected on the number of same-day surgeries performed, emergency visits, and readmission rates. Patient-reported measures were collected using a voluntary online survey 1 week post-operatively using a validated PREs and recovery from surgery survey. Outcome measures were reported to the regional committees through an online provincial dashboard for feedback to clinical teams.
Results: Development of support materials, assembly of regional committees followed by implementation occurred across the province over 18 months, with final nursing in-services was completed in mid-2017. Regional modifications to aspects of the pathway were made in accordance with local patient population characteristics. Barriers to uptake include lack of surgery-specific nurse navigator support in smaller regions and surgeon preference for overnight admission. Since the initiation and implementation of the perioperative pathway, SDS rates for mastectomy in Alberta have improved from 1.2% to 40% in 2017-2018, releasing an estimated 1031 bed days. One hundred two patients voluntarily completed the PRE survey, with 91% of respondents indicating they felt “excellent or good” with the plan to go home, 93% indicating they felt “excellent or good” about how to take care of themselves once they were home, and 93% indicating they felt “excellent or good” about knowing who to contact or where to get support if there were issues. Subjective recovery 1 week following surgery was assessed using the Quality of Recovery (QoR-15) questionnaire with patients rating their recovery from 0 (poor) to 10 (excellent) across various domains (pain management, ability to eat, sleep, care for themselves, feel in control, general well-being and return to work or usual home activities). The average response across categories 1 week following surgery was 7.9.
Conclusions: Development and regional implementation of a multi-tiered provincial perioperative pathway for breast cancer resulted in higher use of SDS for mastectomy in the early post-implementation period, with favourable patient reported experience measures.
Abstract, Official Proceedings
Implementation of Post-Mastectomy Home Recovery Program in a Large, Integrated Health Delivery System
Authors: Brooke Vuong1, Sharon Chang2, Amanda Graff-Baker3, Mio Yanagisawa4, Michele Knox5, Gillian Kuehner6, Margaret Mentakis7, Lucinda Romero8, Veronica Shim9
Institutions: 1Kaiser Permanente South Sacramento Medical Center, Sacramento, CA, 2The Permanente Medical Group, Fremont, CA, 3The Permanente Medical Group, San Jose, CA, 4University of California, Davis, Sacramento, CA, 5The Permanente Medical Group, Hayward, CA, 6The Permanente Medical Group, Vallejo, CA, 7The Permanente Medical Group, Sacramento, CA, 8The Permanente Medical Group, Santa Rosa, CA, 9The Permanente Medical Group, Oakland, CA
Objective: Nationwide, the incidence of mastectomy and reconstruction in an ambulatory setting has been increasing. Surgical home recovery permits the patient to recuperate in a familiar environment, reduces their risk of nosocomial infections, and optimizes utilization of inpatient resources for higher acuity patients. Studies have shown that in well-selected patient populations, same-day surgery for mastectomy is a safe option. A pilot project was initiated within a large, integrated health system to encourage home recovery of mastectomy patients, including patients undergoing implant-based reconstruction and bilateral mastectomies.
Methods: Surgical Home Recovery Program (SHRP) for mastectomy patients was implemented in October 2017 via a regional breast clinical performance team. The goal was to minimize practice variability across surgeons and medical centers in a large, integrated health care delivery system providing coverage to 4.3 million members. Specific measures included setting patient expectations at the initial consultation, educating patients about postoperative home care, using multi-modality pain management to decrease postoperative nausea and vomiting and pain, and timely post-discharge follow-up with patients by phone or e-mail. SHRP included the entire surgical team from breast care coordinators to post-anesthesia care unit recovery nurses. Providers received monthly reports on regional and medical center specific rates of home recovery following mastectomy, in order to share and implement best practices. All patients undergoing mastectomy, including those undergoing immediate implant-based reconstruction and/or double mastectomies, were included. Patients undergoing immediate autologous tissue reconstruction were excluded, as were patients who were hospitalized for >1 day following mastectomy. The primary endpoint was the rate of same day discharge. Chi-square analysis was used to compare the 2 mastectomy cohorts 6 months before and after the implementation period of October 2017 – March 2018. We also compared emergency department (ED) visits, reoperations, and readmissions within 7 days for SHRP patients vs patients who were admitted overnight.
Results: Twenty-one medical centers participated in the regional initiative. Prior to implementing SHRP, 164 of the 628 (26%) of the mastectomies were outpatient procedures. After the implementation period, 403 of the 620 (65%) mastectomies underwent home recovery (p<0.001) [Figure]. Despite the increased rate of outpatient mastectomy, there was no statistically significant differences in presentation to the ED (5.1% vs 5.66%, p=0.67), reoperation (1% vs 2%, p=0.72), or readmission (.8% vs 1.9%, p=0.08).
Conclusions: By implementing standard expectations and sharing best practices, there was a significant increase in the rate of home recovery for mastectomy without compromising quality of patient care. The successful implementation of this pilot program supports expansion of the surgical home recovery program for all patients undergoing mastectomy.