View the up-to-date information for the 2026 Annual Meeting.

Press Release
Contact
Molly McDougall/
Jeanne-Marie Phillips
HealthFlash Marketing
203-977-3333
molly@healthflashmarketing.com
Sharon Grutman
The American Society of Breast Surgeons
877-992-5470
sgrutman@breastsurgeons.org
Download
Intraoperative Lymph Node Pathology Evaluation May Lead to Over-Treatment of the Axilla in Mastectomy Patients
New Study Links Axillary Management Decisions Made During Surgery to Aggressive Treatment of Patients with Limited Nodal Disease
Abstract: Intraoperative Pathology Assessment May Lead to Overtreatment of the Axilla in Clinically Node-Negative Breast Cancer Patients Undergoing Upfront Mastectomy
Columbia, MD, April 27, 2023—Patients who underwent pathology evaluation of their sentinel lymph nodes (SLN) during mastectomy surgery were significantly more likely to receive aggressive nodal therapy than women whose lymph node biopsies and treatment strategies were evaluated post-surgically, according to a study presented this week at the American Society of Breast Surgeons Annual Meeting in Boston. The research focused on mastectomy patients who had tumors up to 5cm, presented as clinically node-negative (without observable symptoms), did not receive any pre-surgical treatment and were found on SLN biopsy to have one or two positive nodes.
“This large national study is notable because it provides evidence that a significant percentage of the mastectomy patients with limited disease in up to two SLNs may be over-treated with axillary node dissection (ALND) (surgical removal of nodes under the arm) or a combination of both ALND and post-surgical axillary radiation therapy (AxRT) simply because their pathology results are read and acted on while the they are on the operating table,” comments study senior author Olga Kantor, MD, MS, Breast Surgical Oncologist at Brigham and Women's Hospital and Dana-Farber Cancer Institute and Assistant Professor of Surgery, Harvard Medical School. SLN biopsies are typically performed during mastectomy procedures, but timing of results interpretation is variable. By contrast, for lumpectomy, results are typically interpreted after surgery.
Although potentially avoiding a second surgery of the axilla, the study suggests that intraoperative pathology assessment influences ALND decision-making, which often does not take place in the context of the patient’s overall treatment plan that may include radiation. This leads some women to receive both therapies.
Dr. Kantor notes that for a similar mastectomy patient population with limited nodal disease, the AMAROS clinical trial found that ALND and AxRT provide excellent and comparable axillary control. “However, radiotherapy is often preferable because it avoids surgical morbidities, including debilitating lymphedema. Moreover, in some cases of micrometastatic nodal disease, patients may avoid both procedures with just ongoing observation of the axilla.”
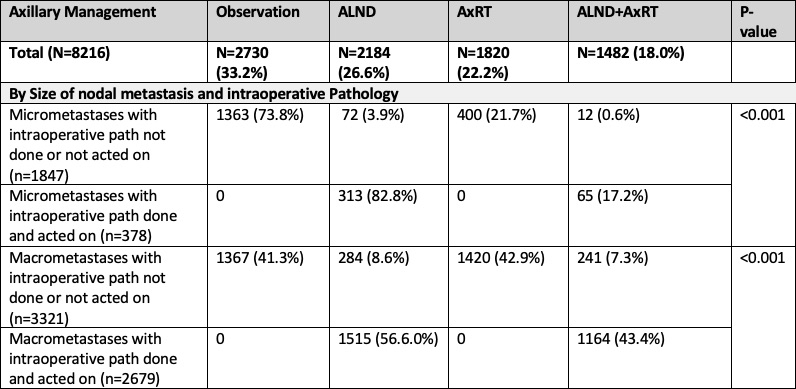
“We conducted this study to assess the impact of the two practice patterns in a large mastectomy patient cohort,” says Dr. Kantor. Examining the National Cancer Database from 2018-2019, researchers identified 8,216 AMAROS-eligible breast cancer patients (with tumors up to 5cm and clinically node-negative) who met all study criteria and underwent mastectomy. Intraoperative pathology was not performed or acted on in 5,159 or 62.8% of cases and performed and acted upon in 3,057 or 37.2% of women. Overall axillary management was observation in 2,730 (33.2%), ALND in 2,184 (26.6%), AxRT in 1,820 (22.2%), and ALND+AxRT in 1,482 (18.0%).
On a multivariate analysis adjusting for patient and tumor characteristics, intraoperative pathology assessment and real-time axillary surgical decision-making was the strongest predictor of whether a patient ultimately received both ALND and AxRT – not clinical criteria such as an increasing number of positive lymph nodes or the size of nodal metastases.
In the study, 40.2 % of women (43.4% of women with macrometastases and 17.2% with micrometastases) were treated with both ALND and AxRT following intraoperative pathology assessment. Only 4.9% (7.3% with macrometastases and 0.6% with micrometastases) were similarly treated with post-operative pathology interpretation and decision-making. Notably, only a small percentage of patients returned to the operating room for ALND when pathology was considered after mastectomy surgery.
“The results of the study are clear – a large number of women are potentially being over-treated when axillary management decisions are made intraoperatively,” comments Dr. Kantor. “Notably, post-surgical decisions typically involve a multi-disciplinary team, including radiation oncologists, which will likely result in a more integrated overall treatment plan. This study suggests that surgeons should delay ALND decision-making until a later time to avoid over-treating patients.”
Abstract, Official Proceedings
Intraoperative Pathology Assessment May Lead to Overtreatment of the Axilla in Clinically Node-Negative Breast Cancer Patients Undergoing Upfront Mastectomy
Authors: Robert Pride1, Charity Glass2, Faina Nakhlis3, Alison Laws4, Anna Weiss3, Jennifer Bellon3, Elizabeth Mittendorf4, Tari King4, Olga Kantor4
Institutions: 1Massachusetts General Hospital/Brigham and Women's Hospital/Dana Farber Cancer Institute, Brookline, MA, 2Massachusetts General Hospital/Brigham and Women's Hospital/Dana Farber Cancer Institute, Boston, MA, 3Brigham and Women's Hospital/Dana Farber Cancer Institute, Boston, MA, 4Dana Farber-Cancer Institute/ Brigham & Women's Hospital, Boston, MA
Background/Objective
Randomized trials have established the safety of observation or axillary radiation (AxRT) as an alternative to axillary lymph node dissection (ALND) among patients with limited nodal disease who undergo upfront surgery. While omission of ALND has been widely accepted for clinically node-negative patients found to have 1-2 positive sentinel lymph nodes (SLN) who undergo breast conserving surgery, variability remains with regards to axillary management in similar patients undergoing mastectomy. Intraoperative pathology assessment can influence decision making about ALND in the operating room and may lead to increased use of both ALND and AxRT in mastectomy patients otherwise eligible for axillary management with either approach per the AMAROS trial; this may be considered axillary overtreatment and translate to increased morbidity. Here we examine the impact of intraoperative pathology assessment in axillary management in a large cohort of AMAROS-eligible mastectomy patients reported to the National Cancer Database (NCDB).
Methods
The NCDB was used to identify AMAROS eligible cT1-2N0 breast cancer patients from 2018-2019 undergoing upfront mastectomy and SLN biopsy (SLNB) found to have 1-2 positive SLN. We examined axillary management patterns by size of nodal metastases and use of intraoperative pathology. Intraoperative pathology assessment was defined as either “not done/not acted on” if ALND was either not performed or performed at a later date than SLNB, or “done/acted on” if SLNB and ALND were performed on the same day. AxRT was defined as postmastectomy radiation including radiation to the draining lymph nodes. Adjusted multivariable analysis was used to examine predictors of receiving both ALND+AxRT.
Results
Of 40,467 patients with cT1-2N0 disease who underwent upfront mastectomy that would be AMAROS-eligible, 8,216 (20.3%) had 1-2 positive SLN. Intraoperative pathology was not done/not acted on in 5,159 (62.8%) cases and done/acted on in 3,057 (37.2%). Overall axillary management was observation in 2,730 (33.2%), ALND in 2,184 (26.6%), AxRT in 1,820 (22.2%), and ALND+AxRT in 1,482 (18.0%).
Patients with intraoperative pathology acted on were significantly more likely to have both ALND+AxRT than those without intraoperative pathology (17.2% vs 0.6% for micrometastases; 43.4% vs 7.3% for macrometastases, both p< 0.001). Axillary management by size of nodal metastasis and intraoperative pathology is shown in the Table. In those patients with intraoperative pathology not done/not acted on, 609 (11.8%) returned to the operating room for ALND.
On multivariate analysis adjusting for patient features and tumor characteristics, the strongest predictor of receiving both ALND+AxRT was use of intraoperative pathology (OR 8.53, 95% CI 7.32-9.95, p< 0.001). Additional predictors included macrometastases (OR 3.45) and increasing number of total positive nodes (OR 2.11 for 2, OR 3.84 for 3, OR 5.41 for >3).
Conclusions
In a large population of AMAROS-eligible cT1-2N0 patients undergoing upfront mastectomy with 1-2 positive SLN, acting on intraoperative pathology significantly increased the use of both ALND+AxRT. Omission or selective use of intraoperative pathologic assessment in this population would encourage consideration of AxRT as an alternative to ALND when appropriate to minimize axillary overtreatment and associated morbidity.