View the up-to-date information for the 2026 Annual Meeting.

Press Release
Contact
Molly McDougall/
Jeanne-Marie Phillips
HealthFlash Marketing
203-977-3333
molly@healthflashmarketing.com
Sharon Grutman
The American Society of Breast Surgeons
877-992-5470
sgrutman@breastsurgeons.org
Download
Exercise and Wellness Programs Enhance Breast Cancer Patients’ Well-Being and Can Lower Healthcare Costs
New Studies Show Significant Impact of Prehabilitation and Post-Surgical Programs
Abstract: The Benefits of a Clinically Based Individualized Exercise Oncology Program on Quality of Life and Health Care Costs for Early-Stage Breast Cancer Patients
Abstract: A Randomized Control Pilot of Prehabilitation During Neoadjuvant Chemotherapy for Women with Breast Cancer: A Mixed Methods Study
Columbia, MD, April 27, 2023—Specialized exercise and wellness programs significantly elevated breast cancer patients’ physical well-being and quality-of-life while reducing healthcare costs in new research presented this week at the American Society of Breast Surgeons Annual Meeting in Boston.
Karen Wonders, PhD, FACSM, lead study author and Professor of Exercise Physiology, Program Director of Exercise Science at Wright State University, and her team examined the impact of a 12-week post-surgical program of individualized exercise aligned with the American College of Sports Medicine Guidelines for Cancer Survivors. They found program participants improved on all health-related quality-of-life measurements, while the control group declined or remained the same. Also examining for the first time the relationship between exercise intervention and utilization of healthcare resources, researchers found that patient emergency department (ED), hospital and office-based visits significantly declined, lowering healthcare costs.
Canadian researchers, led by Frances Wright, MD, MEd, FRCSC, lead study author and Professor of Surgery at Sunnybrook Health Sciences Center, Toronto, ON, presented data on the impact of individualized prehabilitation programs combining exercise with dietary and stress management counseling on breast cancer patients prior to surgery as they underwent neoadjuvant (pre-surgical) chemotherapy (NACT). Immediately after chemotherapy and six months post-cancer surgery, program participants demonstrated better functional walking capacity and self-reported general quality-of-life and fatigue measurements as well as other improvements compared to the control group.
Dr. Wonders’ prospective clinical trial involved 243 patients randomized to the exercise and control groups. Interventions consisted of 150 minutes of cardiovascular exercise weekly, primarily walking or recumbent bicycling at a low to moderate intensity. Each week, the group also engaged in two to three 60-minute sessions of full body workouts weekly using free weights or exercise stretch bands.
Both groups were assessed pre- and post-intervention using the Functional Assessment of Cancer Therapy-Breast (FACT-B), the Short Form-36 Health Survey (SF-36) and the Brief Fatigue Inventory (BFI).
“These well-recognized measurement tools focus on physical, social, emotional and functional well-being, rating performance on a scale of one to 28. Controlling for demographic factors and comorbidities, differences between the two groups were significant,” comments Dr. Wonders. “There was a linear relationship between exercise and decrease in health care utilization.” ED visits decreased by 33.2%, hospital outpatient visits by 21.5% and office-based visits by 41.8%.
“With a growing recognition of the importance of exercise, currently it is written into the standards or guidelines of several major national U.S. breast cancer organizations,” she comments. “Our study adds to the body of literature supporting it, not only by demonstrating benefits but also by showing that exercise can help cut healthcare costs.”
Dr. Wright’s research breaks new ground in examining prehabilitation (a program focused on optimizing health during the pre-operative time period) for breast cancer patients as they embark on a stringent course of varied of cancer therapies for up to 12 months. While the main aim of the study was to assess the feasibility of such a program, the study also yielded significant data on its benefits. With almost half of the women approached agreeing to participate and 87% completing the program, authors conclude that prehabilitation is feasible and well-received by patients.
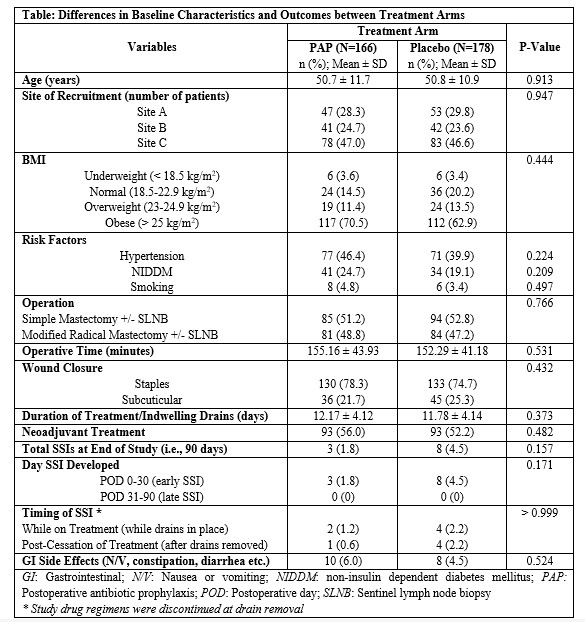
In the study, 72 participants were randomized into the intervention and control groups. The attrition rate over the course of the study was 13%. Prehabilitation consisted of an individual counseling session with a nutritionist and psychiatrist. After evaluation by a physiotherapist, participants were assigned a customized exercise program centering on several 30-minute cardiovascular exercise sessions each week complemented by upper body strength training.
They were administered physical fitness tests and a variety of well-recognized self-rating health-related questionnaires for baseline, post-NACT and post-surgical data. In addition to these quantitative measures, qualitative interview data suggested that the program had a substantial positive impact on the treatment experience overall.
“The impact of our prehabilitation was quite positive with no intervention-related adverse events reported,” comments Dr. Wright. “While a more extensive trial is warranted to determine efficacy, our program will be operationalized shortly though a non-profit that will offer it on a virtual platform nationally throughout Canada for women who wish to participate. We are very excited about the prospects.”
Both researchers agree that exercise and wellness programs for breast cancer patients are a win-win.
Abstract, Official Proceedings
The Benefits of a Clinically Based Individualized Exercise Oncology Program on Quality of Life and Health Care Costs for Early-Stage Breast Cancer Patients
Authors: Karen Wonders1, Kathryn Schmitz2, Jay Harness3, E Ronald Hale4, Arthur Lerner5
Institutions: 1Maple Tree Cancer Alliance, Dayton, OH, 2University of Pittsburgh School of Medicine, Pittsburgh, PA, 3Maple Tree Cancer Alliance, Santa Barbara, CA, 4Kettering Cancer Care, Kettering, OH, 5Maple Tree Cancer Alliance, Palm City, FL
Background/Objective
In 2018, 1.74 million individuals were diagnosed with cancer in the US. The direct and indirect cost of cancer care was $158 billion. Unplanned hospitalizations and ED visits account for a significant portion of overall cancer care costs. Physical and psychosocial interventions have proved efficacious for helping relieve patient burdens and reduce overall costs. The purpose of the present study was to prospectively establish the influence of quality of life on the health care utilization and costs following a 12-week individualized exercise intervention in patients with early-stage breast cancer.
Methods
For this open-label, randomized, prospective, comparative clinical trial, patients with early stage breast cancer (stage I to II) were randomly assigned into two groups: the control group (CG, n =120) and the exercise training group (EX, n = 123). Patients in the exercise intervention group completed 12 weeks of prescribed, individualized exercise that aligned with the American College of Sports Medicine (ACSM) exercise guidelines for cancer survivors. The control group received the current standard of care, which includes a resource guide with various options available to cancer survivors. Both the EX and CG completed the Functional Assessment of Cancer Therapy-Breast (FACT-B), the Short Form-36 Health Survey (SF-36), and the Brief Fatigue Inventory (BFI) at baseline and following the 12-week exercise intervention.
Results
In analysis of covariance models controlling for demographic factors and comorbidities, the breast cancer-specific quality of life improved significantly across categories of each health-related quality of life items in the EX-group as compared to the CG (p< 0.001). In Cox regression models controlling for the same covariates, all of the health-related quality of life questions studied were significant predictors of emergency room (ED) visits, hospital outpatient visits, and private office-based visits. Specifically, ED visits decreased by 33.2%, hospital outpatient visits decreased by 21.5%, and private office-based visits decreased by 41.8%.
Conclusions
These results signify that all dimensions of health-related quality of life items studied were positively impacted by exercise and can be used as indicators to decrease health care costs among patients with early-stage breast cancer. As key providers of breast cancer care, breast surgeons can be important advocates for referring patients to supervised exercise oncology programs.
Abstract, Official Proceedings
A Randomized Control Pilot of Prehabilitation During Neoadjuvant Chemotherapy for Women with Breast Cancer: A Mixed Methods Study
Authors: Priya Brahmbhatt1, Nicole Look Hong2, Apishanthi Srikandarajah2, Sharon Lemon-Wong2, Nasrin Alavi2, Leslie Gibson2, David Berger-Richardson2, Tracey Rapier2, Joanna Mascarenhas2, Elie Isenberg-Grzeda2, Sarah Selvadurai3, Daniel Santa Mina1, Frances Wright2
Institutions: 1University of Toronto, Toronto, ON, Canada, 2Sunnybrook Health Sciences Centre, Toronto, ON, Canada, 3Toronto Western Hospital, University Health Network, Toronto, ON, Canada
Background/Objective
Prehabilitation in other disease settings has demonstrated efficacy in improving peri-operative outcomes. Little is known about the feasibility of multimodal prehabilitation during neoadjuvant chemotherapy (NACT) in women with breast cancer, and whether it can attenuate treatment-related decrements. We hypothesized the prehabilitation during NACT would be feasible and that it would mitigate functional and psychosocial decline during and after NACT.
Methods
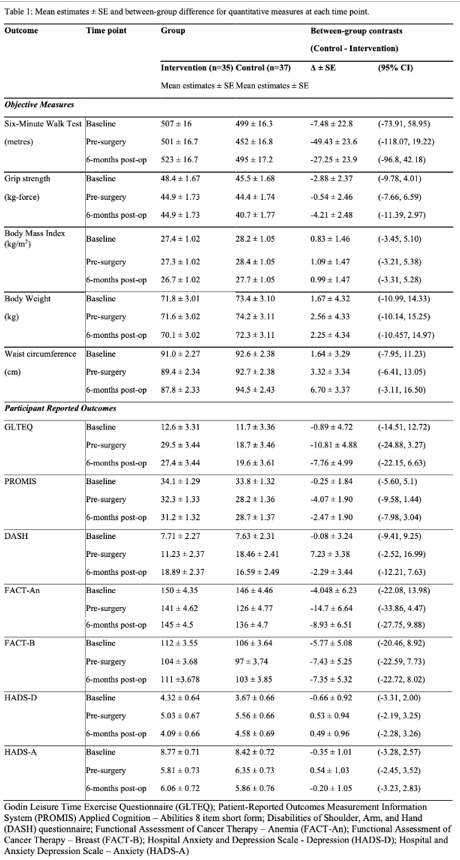
We conducted a multi-site randomized controlled trial of multimodal prehabilitation versus usual care during NACT women diagnosed with non-metastatic breast cancer in Toronto, CA (Sunnybrook Health Sciences Centre and University Health Network). Participants in the prehabilitation group received an individualized exercise program for the duration of NACT, dietetic support, and stress management counselling. Feasibility metrics included recruitment rates, attrition, and intervention-related adverse events. We also conducted an exploratory analyses of intervention efficacy on physical fitness (six-minute walk test, grip strength, anthropometrics) and psychosocial outcomes (participant-reported quality of life, fatigue, physical activity levels, upper quadrant function, and anxiety and depression) using linear mixed effects models. Data were collected before initiating NACT, following NACT completion, and six months after surgery. We also conducted semi-structured interviews in a subset of participants after study completion to understand their prehabilitation experiences more comprehensively. These data were analyzed using inductive thematic analysis.
Results
A total of 137 women were approached across the two study sites. Of these, 72 were randomized, resulting in a recruitment rate of 53%. There was an attrition rate of 13% over the study period. Mean participant age was 54.2 years (standard deviation [SD]: 11.48 years) and participants received an average of eight NACT cycles (range: 4 – 12). There were no intervention-related adverse events reported. Participants in the prehabilitation group were meeting physical activity guidelines based on self-reported physical activity at both post-chemotherapy time-points whereas control participants were not.
Participants in the prehabilitation group had better functional walking capacity at the post-chemo time-point (between group difference of 49.43 m ± SD 23 m; 95% confidence interval [CI]: -118.07, 19.22) and at the post-surgery time-point (27.25 ± SD 23.9; 95% CI: -96.8, 42.18) compared to the control group. Intervention participants also reported better quality of life and less fatigue when compared with controls at both post-NACT timepoints (values represented clinically important differences). The qualitative data from the interviews (n=six) suggested that the intervention had a substantial positive impact on the treatment experience. Major themes that emerged from the interviews included: i) the diagnosis period as being extremely overwhelming; ii) prehabilitation as education; and iii) prehabilitation as respite. Other important themes included barriers and facilitators to prehabilitation participation and other unfulfilled needs from prehabilitation.
Conclusions
Prehabilitation during NACT in women with breast cancer is feasible and well received. Our pilot study suggests that multimodal prehabilitation may improve clinically relevant outcomes including physical fitness, quality of life, and fatigue. An adequately powered trial to determine efficacy is warranted.